

We are focused on developing and delivering innovative therapies for the treatment of liver and cardiometabolic diseases. Our lead candidate, pegozafermin, is currently being developed for the treatment of MASH and SHTG.
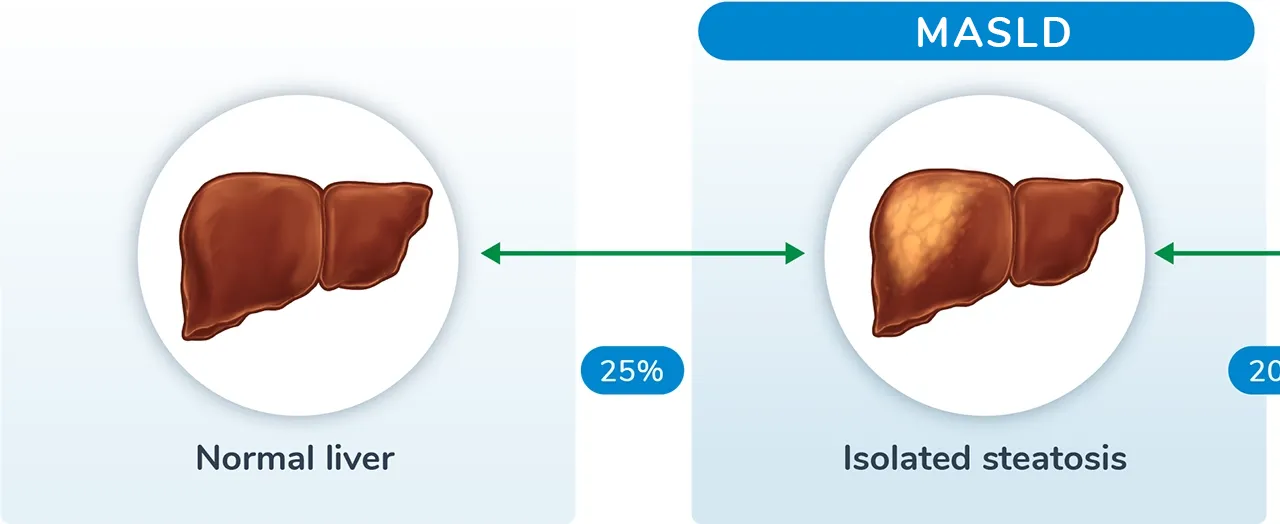
MASH is a severe form of metabolic dysfunction-associated steatotic liver disease (MASLD) defined by liver inflammation and injury. The disease progresses over time, resulting in increased fat accumulation in the liver and, in many cases, permanent scarring of the liver.
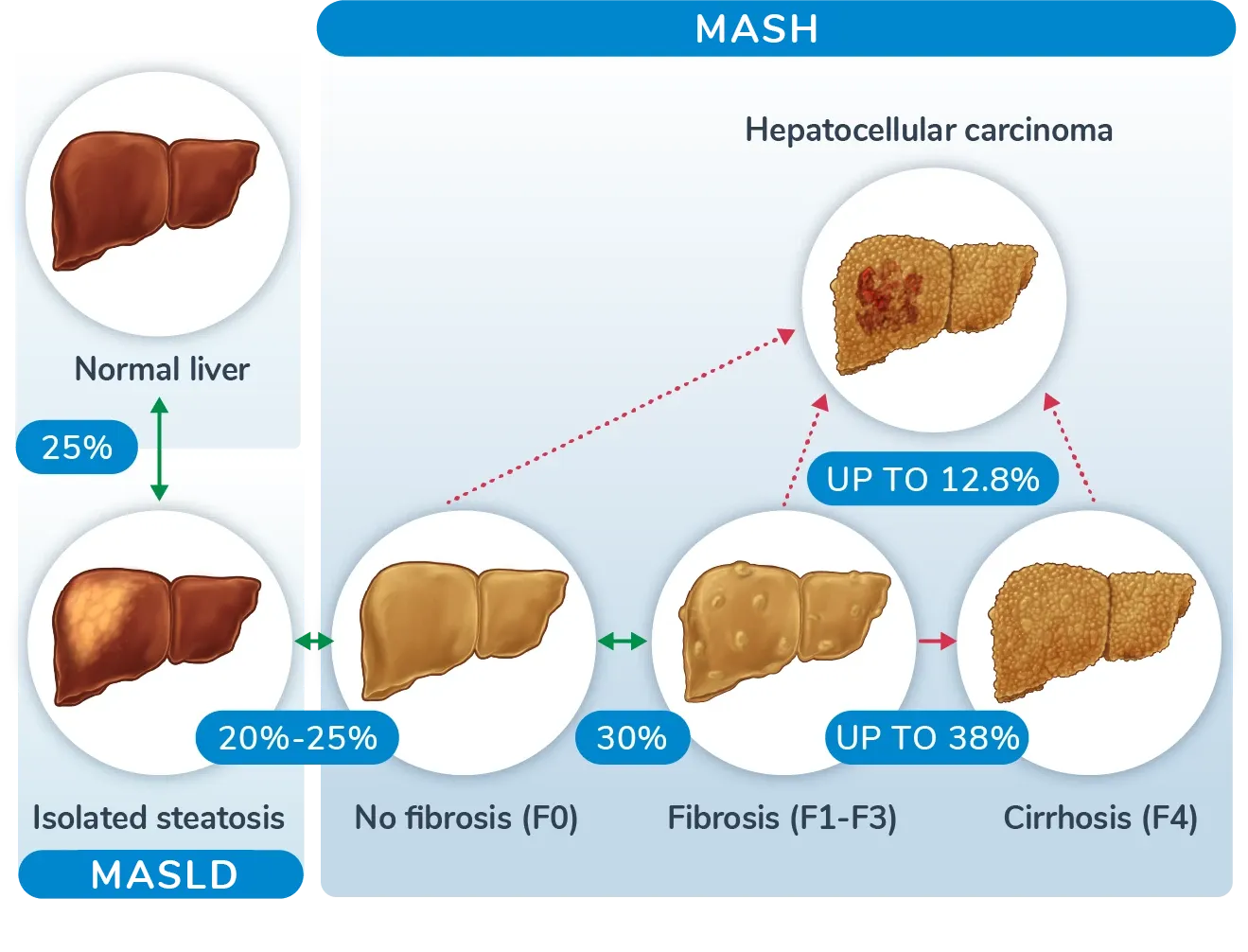
MASH is a severe form of metabolic dysfunction-associated steatotic liver disease (MASLD) defined by liver inflammation and injury. The disease progresses over time, resulting in increased fat accumulation in the liver and, in many cases, permanent scarring of the liver.
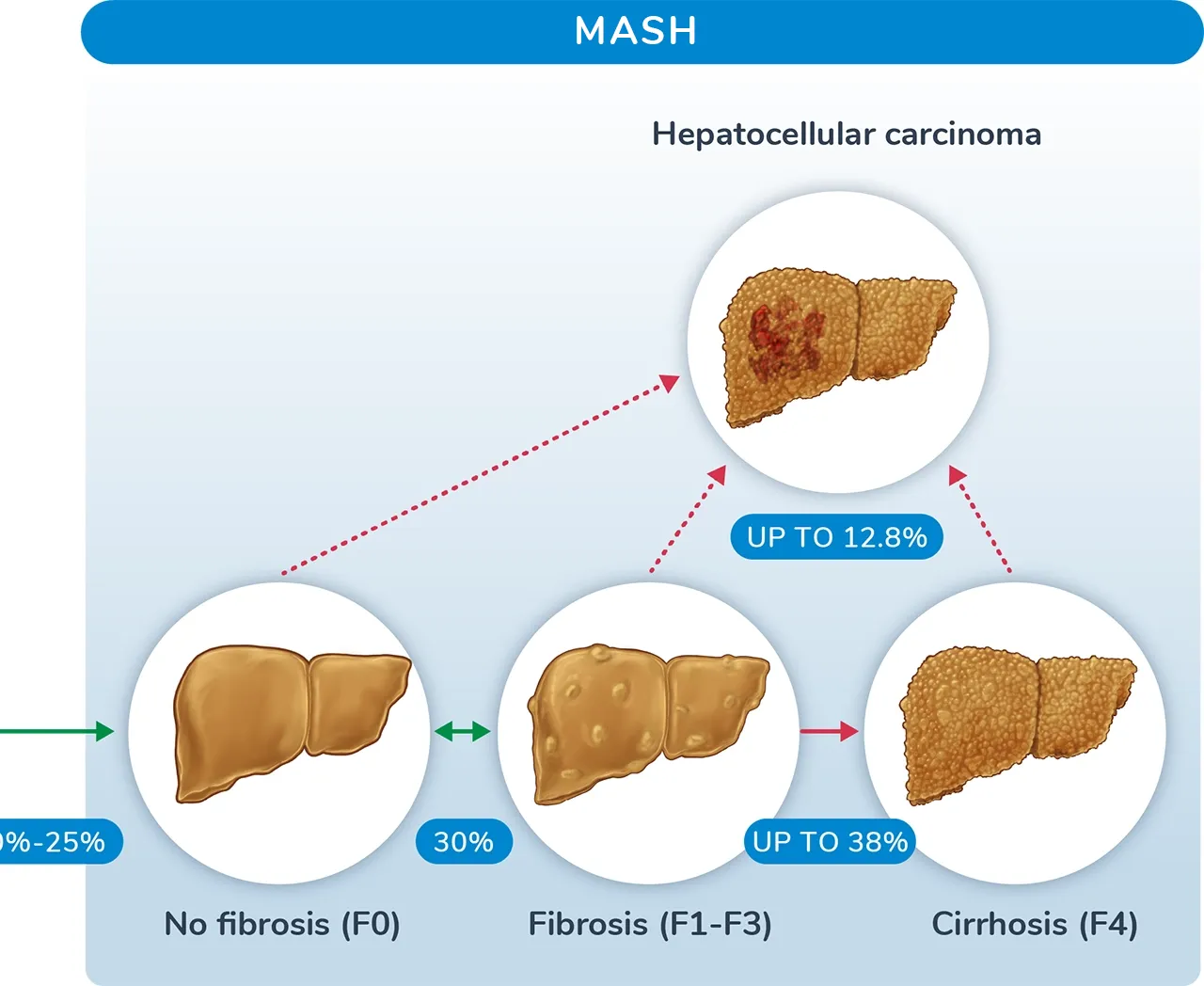
MASH progression can result in cirrhosis, liver failure, liver cancer, and death. In fact, MASH is the second leading cause of liver transplant among all adults, and it is expected to become the dominant cause for liver transplant in coming years. In addition, MASH predicts risk of cardiovascular events, and the presence of MASH increases the risk of cardiovascular disease above that of MASLD.
The majority of patients with MASH have been diagnosed with other cardiometabolic comorbidities:




The occurrence of comorbidities increases with progression from MASLD to MASH.
In the US, approximately 25% of the population will develop MASLD, with 20-25% of those patients progressing to MASH. The prevalence of MASH in the US is predicted to increase 63% from 16.5 million cases in 2015 to 27.0 million cases in 2030, with similar rates across Europe.
MASH develops through fat accumulation in the liver which often leads to insulin resistance. These two factors can result in increased inflammation and cellular injury within the liver. The inflammation then promotes the secretion of excess collagen, causing the fibrosis, or scarring, of the liver.

The primary treatment goal for MASH is to reduce fibrosis in the liver, which we believe to be a major predictor of poor clinical outcomes. Current treatment approaches target other metabolic disorders and are insufficient at addressing liver fibrosis. Our treatment goals for MASH are improved fibrosis and MASH resolution, as well as improvement in metabolic parameters.
SHTG is a lipid abnormality defined by severely elevated triglyceride (TG) levels, with fasting TG levels ≥500 mg/dL. SHTG can result from environmental factors, such as poor diet, and, less frequently, genetic conditions, such as familial chylomicronemia, that cause an imbalance between TG production and breakdown. Persistent elevation of TG levels can ultimately result in abnormal fat deposition in organs throughout the body, including the liver, pancreas, heart, and muscle, potentially leading to lipotoxicity and insulin resistance.
The risk for severe diseases like acute pancreatitis and atherosclerotic cardiovascular disease (ASCVD) increases as TG levels increase. Both acute pancreatitis and ASCVD have life-threatening consequences and can lead to organ failure and death.






*Patients with TG levels ≥2000 mg/dL.
SHTG currently affects ~2% of the US population, but the number of patients with SHTG is expected to rise due to the increasing prevalence of obesity and diabetes. Over the next decade, nearly 3.4 million ASCVD events, such as heart attack or stroke, are expected to occur among patients with elevated TG levels, highlighting the need for treatments that can reduce TG levels and provide broad metabolic benefits for patients.
SHTG is an asymptomatic disorder that often goes untreated, with only 20% of patients currently on medication, including statins, fibrates, and fish oils. These SHTG treatment options can help reduce TG levels, but they often have tolerability issues and are often insufficient for improving liver and cardiometabolic comorbidities, which is the goal of treatment for SHTG.

Insulin resistance leads to the secretion of free fatty acids and, over time, inflammation. Low-grade inflammation caused by SHTG may lead to the release of free fatty acids in the pancreas. This, in turn, leads to a cycle of continuing inflammation and, ultimately, acute pancreatitis events. At the same time, elevated TGs in circulation ultimately lead to a more atherogenic lipid profile resulting in increased arterial inflammation and plaque formation, promoting the progression of ASCVD.
1. Younossi ZM, et al. Hepatology. 2016;64(1):73-84. 2. Iqbal U, et al. Medicines. 2019;6(1):41. 3. Estes C, et al. Hepatology. 2018;67(1):123-133. 4. Loomba R, et al. Cell. 2021;184:2537-2564. 5. Cusi K. Gastroenterology. 2012;142(4):711-725. 6. Sanyal AJ, et al. N Engl J Med. 2021;385(17):1559-1569. 7. Angulo P, et al. Gastroenterology. 2015;149(2):389-397. 8. Loomba R, et al. Hepatology. 2019;70(6):1885-1888. 9. Younossi ZM, et al. Clin Gastroenterol Hepatol. 2021;19(3):580-589. 10. Wong RJ, Singal AK. JAMA Netw Open. 2020;3(2):e1920294. 11. Ratziu V, et al. J Hepatol. 2015;62(1 Suppl):S65-S75. 12. Chalasani N, et al. Hepatology. 2018;67(1):328-357. 13. Virani SS, et al. J Am Col Cardiol. 2021;78(9):960-993. 14. Hansen SEJ, et al. Clin Chem. 2019;65(2):321-332. 15. Murphy MJ, et al. JAMA Intern Med. 2013;173(2):162-164. 16. Perry AF, et al. Gastroenterol. 2012;143:1179-1187. 17. Tenner S, et al. Gastroenterol. 1997;113:899-903. 18. Toth PP. Vasc Health Risk Manag. 2016;12:171-183. 19. Peng J, et al. Lipids Health Dis. 2017;16(1):233. 20. Nordestgaard BG, et al. JAMA. 2007;298(3):299-308. 21. Miller M, et al. Circulation. 2011;123(2):2292-2333. 22. Bhatt DL, et al. Prevalence of Nonalcoholic Fatty Liver Disease in Patients with Severe Hypertriglyceridemia (SHTG) – Initial Baseline Data From an Ongoing Phase 2 Study. Poster presented at: 16th Annual Cardiometabolic Heath Congress; October 14-17, 2021; National Harbor, MD. 23. Retterstøl K, et al. Lipids Health Dis. 2017;16(1):1-8. 24. Christian JB, et al. Am J Card. 2011;107(6):891-897. 25. Esparza MI, et al. J Endocr Soc. 2019;3(8):1595-1607. 26. Karanchi H, et al. StatPearls; 2022. 27. Fan W, et al. J Clin Lipid. 2019;13:100-108. 28. Jellinger PS, et al. Endocr Pract. 2017;23(4):479-497. 29. Semova I, Biddinger SB. Trends Pharmacol Sci. 2021;42(3):183-190. 30. Sandesara PB, et al. Endocr Rev. 2019;40:537-557.